Enteral Feeding Basics: What Home Carers Need to Know About Tube Care

If you’re caring for someone with a feeding tube, first of all — take a deep breath. You’re doing something incredibly important, and yes, it can feel overwhelming at first. But with a little know-how and the right tools, enteral feeding doesn’t have to be scary or complicated.
Whether it’s a PEG, NG, or another type of tube, enteral feeding is simply a way of delivering nutrition directly to the stomach or small intestine. It’s used when someone can’t eat enough (or at all) by mouth — but still needs all the nourishment their body depends on.
This guide is here to help you understand the basics of tube feeding, what supplies you’ll need, how to keep everything clean and safe, and how to spot issues before they become bigger problems.
Common Tube Types and What They Do
If you’ve ever looked at a feeding tube and quietly thought, “I hope I’m doing this right,” — you’re not alone. Tube care can feel intimidating at first, especially when you’re not a nurse. But once you understand the different types and what they’re for, it all starts to make a lot more sense.
Let’s break down the most common types of feeding tubes carers are likely to come across — and what you need to know about each.
1. Nasogastric (NG) Tube
What it is:
A thin, flexible tube that goes through the nose and down into the stomach. It’s often used for short-term feeding (usually a few weeks), particularly after surgery or during recovery from illness.
Key features:
- Easy to place and remove without surgery
- Typically secured with tape on the cheek or nose
- May be used for feeding, hydration, or medication
According to the Cleveland Clinic, NG tubes are commonly used in hospital settings and for patients who only need support for a short time.
What carers should know:
Make sure the tape is secure and that the tube isn’t pulling — movement can cause discomfort or dislodgement. Always follow instructions on how to flush the tube before and after feeds or medications.
Need an NG Tube? Try the CORFLO® 8FR NG Feeding Tube with ENFit® Connector.

This NG tube is designed for safe and secure short-term feeding with ENFit® compatibility, reducing misconnection risks and simplifying daily care.
2. Gastrostomy Tube (PEG or G-Tube)
What it is:
A tube that’s surgically placed directly through the abdomen into the stomach. "PEG" stands for Percutaneous Endoscopic Gastrostomy — a common method of placing a G-tube.
Key features:
- Used for long-term feeding (months to years)
- Held in place by an internal bumper or balloon
- Feeds go straight into the stomach
As outlined in NCBI Clinical Guidelines, PEG tubes are suitable for patients who need ongoing nutritional support but still have functioning digestive systems.
What carers should know:
Site care is important — clean around the insertion point daily and check for redness or discharge. If the tube feels loose or leaks around the site, get clinical advice.
Need a G-Tube? Try the MIC-G Balloon Gastrostomy Feeding Tube with ENFit® Connectors.
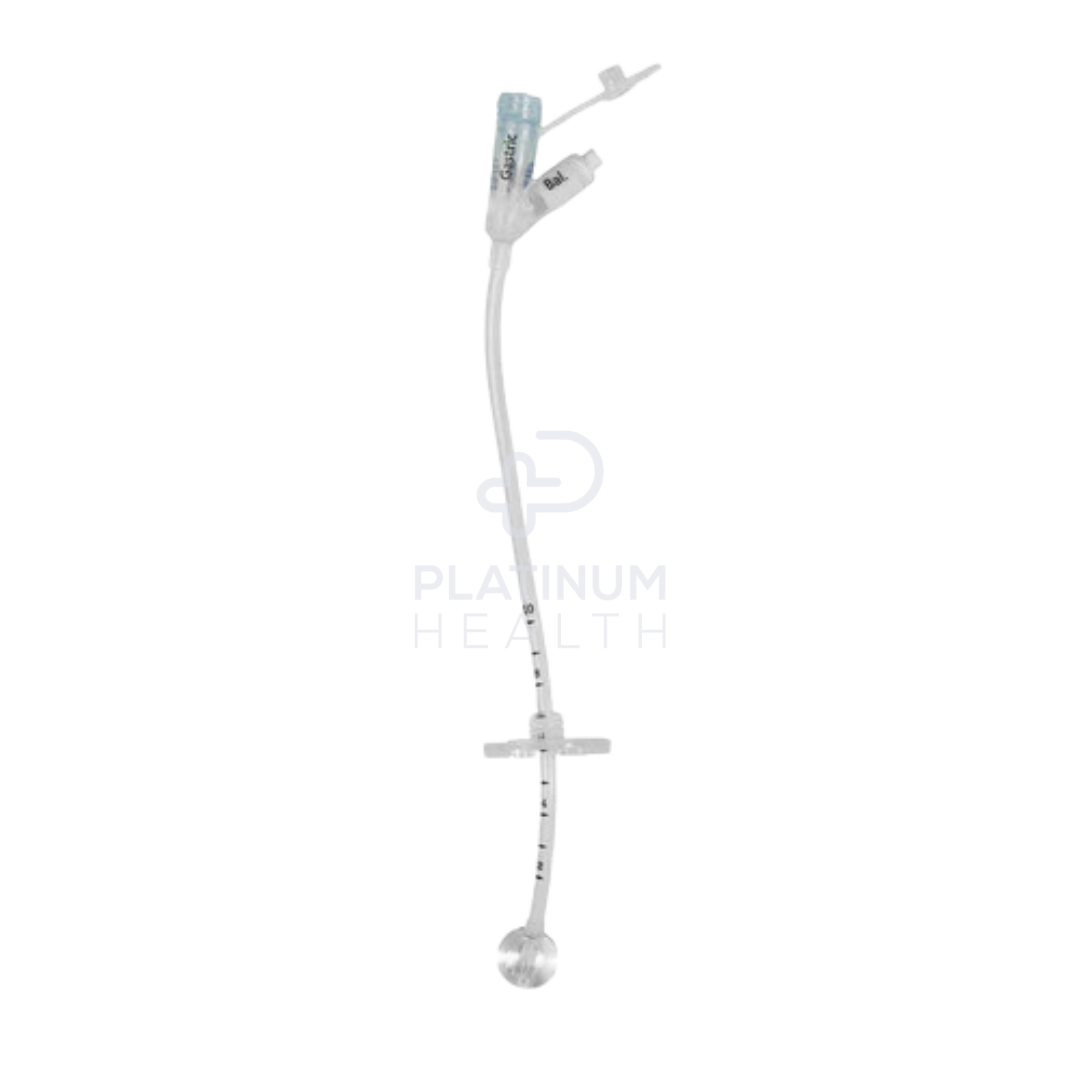
This low-profile G-tube is ideal for long-term use and features ENFit® connectors for added safety and a balloon for secure internal retention.
3. Jejunostomy Tube (J-Tube)
What it is:
A feeding tube placed directly into the jejunum (part of the small intestine), typically when the stomach needs to be bypassed — such as after certain surgeries or when digestion in the stomach is impaired.
Key features:
- Can be placed surgically or endoscopically
- Delivers nutrition directly into the small intestine
- Often used when there is a high risk of aspiration (food entering the lungs)
The NCBI Nursing Guide to Nutritional Support notes that J-tubes are commonly used when gastric feeding is not tolerated or contraindicated.
What carers should know:
Feeds often need to be slower and continuous using a pump, rather than bolus feeds. Always monitor for bloating, diarrhoea, or signs of discomfort, and keep the area clean and dry.
We currently don’t supply J-Tubes at the time of writing this article. However, you might want to consider the MIC-KEY Low Profile Continuous Feed Extension Set with ENFit® Connectors.

While not a J-tube itself, this ENFit-compatible extension set is designed for patients using low-profile Jejunal or Gastro-jejunal tubes — making continuous feeds easier and safer to manage.
Quick Reference Summary
|
Tube Type |
Placement |
Used For |
Best Suited For |
|
NG Tube |
Nose → Stomach |
Short-term feeding |
Post-surgery, recovery |
|
PEG/G-Tube |
Abdomen → Stomach |
Long-term feeding |
Stable, chronic conditions |
|
J-Tube |
Abdomen → Small Intestine |
Stomach bypass |
Aspiration risk, severe reflux |
Daily Tube Care: Cleaning, Flushing & What to Watch For
If you're supporting someone with a feeding tube, daily care becomes part of the routine — like brushing teeth or making breakfast. It might feel a little daunting at first, but once you understand the key steps, it becomes second nature.
The goal? Prevent infection, keep the tube working properly, and help your loved one stay comfortable.
1. Cleaning Around the Tube Site (PEG/G-Tube or J-Tube)
Cleanliness is essential — especially where the tube enters the skin.
According to Queensland Health, the stoma (the opening where the tube enters the body) should be cleaned at least once a day using warm water and a clean cloth or gauze.
Here’s how to do it:
1. Wash your hands thoroughly.
2. Use clean water (no soap needed unless directed) to gently clean around the stoma site.
3. Pat dry with a clean towel or gauze — no rubbing.
4. Rotate the tube slightly (if advised by a nurse or doctor) to prevent skin sticking.
️
Avoid creams, powders, or ointments unless specifically recommended by a healthcare professional. These can irritate the skin or cause blockage.
For NG tubes, check that the tube is still properly taped in place and hasn’t moved. If the skin on the nose or cheek looks red or irritated, gently adjust the tape and let a healthcare professional know.
2. Flushing the Tube
Flushing the tube keeps it clear of blockages and ensures feeds and medications don’t get stuck.
- Before and after every feed: Flush with warm, sterile water (usually 30–60 mL — check with your care team).
- Before and after giving medication: Flush between each medication to prevent interaction or clogging.
- If the tube is not in constant use: Flush at least once or twice a day to keep it patent.
As TubeFed Australia points out, flushing is one of the most important habits for carers — and skipping it can lead to clogs that require a trip to the hospital.
Always use a 30–60 mL syringe with a gentle push-pause technique, unless directed otherwise.
What to Watch For
Staying alert to changes — even small ones — is one of the best things you can do as a carer. Here are some signs that something might be off:
- Redness, swelling, or discharge around the stoma
- Leaking fluid from the site
- Unusual odours
- Pain or discomfort during feeding
- The tube feels loose or has changed position
- Feeds not flowing properly or resistance when flushing
According to National Jewish Health, any of these could mean the tube is blocked, dislodged, or infected — and it’s best to contact a nurse or doctor promptly.
Quick Tip:
Keep a daily checklist or care log to track feed volumes, flushes, and any changes in the site. It’s a great way to spot patterns and helps a nurse or doctor understand what’s going on if you need support.
Troubleshooting: What to Do If Something Doesn’t Look Right
Feeding tubes are safe and reliable when cared for properly — but even with the best routine, little hiccups can happen. The key is knowing what’s normal, what’s not, and when it’s time to get help.
Here’s what to watch out for — and what you can do about it.
Common Tube Concerns (and What They Might Mean)
1. The tube is leaking at the stoma site
Leaking formula or stomach fluid can irritate the skin and cause infection. It may be a sign the tube has shifted, the internal balloon has deflated, or the stoma has stretched.
What to do:
- Gently clean the area
- Apply a dressing if needed to absorb leakage
- Call your nurse, GP, or home care team — especially if the leak is persistent or smells bad
2. The skin around the tube is red, swollen, or painful
A bit of redness is common, but if the area looks increasingly angry, feels warm, or starts to ooze, it could be the start of an infection.
What to do:
- Keep the area clean and dry
- Don’t apply creams or antiseptics unless directed
- Contact a health professional for assessment — especially if there’s a fever or pain
3. The tube won’t flush or feed won’t go in
Blockages happen — especially if medication wasn’t flushed through properly or feeds were too thick.
What to do:
- Try gently flushing with warm (not hot) water using a 30–60 mL syringe
- Never force it — that can cause damage
- If it’s still blocked, stop and call your care team or go to your local health provider
4. The tube has fallen out or partially come out
This can be a little confronting — but don’t panic. If it’s a G-tube or J-tube and it comes out, the stoma can start to close within hours.
What to do:
- Don’t try to put the tube back in yourself
- Cover the site with a clean dressing or cloth
- Call your doctor or go to the emergency department as soon as possible
If it’s an NG tube that’s come out, it may be able to be reinserted at home by a trained carer or nurse, depending on your care plan.
5. The person is vomiting, bloated, or in pain during or after feeds
This could be a sign of feeding intolerance, infection, or a misplaced tube — especially with J-tubes or continuous feeds.
What to do:
- Stop the feed immediately
- Sit or reposition the person to relieve pressure
- Contact your GP or nurse — and keep a record of when the symptoms started
When to Ask for Help (and Where to Get It)
Caring for someone with a feeding tube is no small task. While this guide offers practical advice, it's important to remember that every person’s needs are different, and sometimes the best thing you can do is reach out to a professional.
If you’re ever unsure about:
- Tube placement or how it’s working
- Unusual symptoms like pain, swelling, or vomiting
- Whether you’re doing things “the right way”
…don’t hesitate to speak to a GP, nurse, dietitian, or home care provider.
Trusted Australian Support Services
Here are a few helpful places to get extra guidance:
- TubeFed Australia – A fantastic resource for Australian carers managing enteral nutrition at home
- Healthdirect Australia – 24/7 nurse advice line: 1800 022 222
- My Aged Care – For support at home, including clinical care, nursing, and equipment funding
- NDIS – For participants needing enteral feeding supplies and support through their plan
- Your hospital discharge team or community health service
Disclaimer
Platinum Health Supply Group is a healthcare supplies provider — we are not a hospital, clinic, or medical authority. This blog is intended for informational and educational purposes only, based on publicly available resources and best-practice care guidelines.
It is not a substitute for professional medical advice, diagnosis, or treatment. Always follow the instructions of your healthcare team and consult them if you have any concerns about a feeding tube, care routine, or the person you support.
You’re Doing an Incredible Job — We’re Here to Help
Providing care at home — especially for someone with a feeding tube — takes patience, compassion, and a willingness to learn. If you’re feeling overwhelmed, you’re not alone. But with the right tools, support, and information, it gets easier.
Whether you’re adjusting to life with enteral feeding or just need a few extra supplies, we’re here to support you. Our team at Platinum Health Supply Group can walk you through products, answer your questions, and help you feel more confident in your care routine.
📍 Visit us in person:
Unit 2/51 Trafalgar Road, Epping VIC 3076
🕘 Open Monday to Friday: 9:00 AM – 5:00 PM
Prefer to shop from home? Browse our full range of feeding tubes, ENFit accessories, syringes, dressings, and more online — with fast, Australia-wide delivery.
Because no carer should feel like they have to figure it all out alone. Let’s make it easier, together.
